Intersecting Cardiovascular and Mental Health Challenges in Bangladesh

Cardiovascular stress and mental stress have emerged as deeply connected public health crises in Bangladesh and around the world. Often invisible yet widespread, they inflict profound harm not only on individuals but also on families, communities, and national economies. Their consequences reach far beyond hospital walls, shaping life in workplaces, schools, and households, and they call for immediate awareness, prevention, and collective action.
Bangladesh today faces a mounting cardiovascular emergency. Heart disease accounts for nearly 34 percent of all deaths in the country, despite the fact that 80 percent of these cases are preventable through lifestyle changes and timely medical intervention. The Business Standard recently reported that cardiovascular diseases claim 283,000 lives annually, with more than half linked to untreated hypertension. One in four adults in Bangladesh suffers from hypertension, yet access to treatment remains inconsistent. This is not an isolated national problem. The World Health Organization estimates that globally, over 1,000 lives are lost every hour to strokes and heart attacks caused by high blood pressure. The American Heart Association’s 2025 report confirms that cardiovascular disease remains the leading cause of death worldwide, responsible for nearly 40 percent of all deaths in the United States and with similar burdens across Asia, Africa, and Europe.
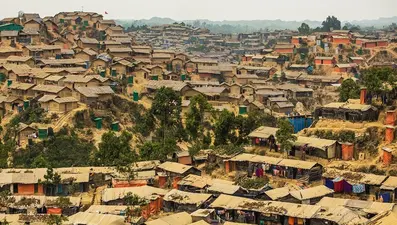
Mental stress is equally alarming. In Bangladesh, rapid urbanization, poverty, overcrowding, and climate vulnerability have created fertile ground for anxiety, depression, and other stress-related disorders. A recent study in Frontiers in Psychiatry found that socio-demographic factors such as poverty, gender inequality, and rural isolation are strongly associated with mental health disorders among women in Mymensingh. Another study in BMC Psychiatry highlighted the treatment gaps in mental health care-seeking behavior, showing that stigma, lack of awareness, and inadequate infrastructure prevent many from accessing care. The National Mental Health Strategic Plan 2020–2030 acknowledges that poverty, environmental stressors, and education are key determinants of mental health in Bangladesh. Globally, the World Health Organization warns that more than one billion people are living with mental health conditions, with anxiety and depression exacting immense human and economic tolls. Mental health problems are now the second leading cause of long-term disability worldwide, costing the global economy an estimated $1 trillion annually in lost productivity.
The socio-public health impacts of these twin stressors are profound. Families in Bangladesh often bear catastrophic medical costs, pushing households into poverty. Productivity losses from absenteeism, reduced work capacity, and premature deaths weaken national economic growth. Children growing up in stressed households face developmental challenges, while employers grapple with declining workforce efficiency. Globally, marginalized communities face higher exposure to stressors and lower access to treatment, perpetuating cycles of disadvantage.
The causes are multifaceted. In Bangladesh, dietary transitions toward processed foods, urban lifestyles with reduced physical activity, and high tobacco consumption fuel cardiovascular stress. Mental stress is driven by economic insecurity, climate shocks, and stigma surrounding mental illness. Internationally, similar causes prevail, though in high-income countries, digital overload, workplace burnout, and social isolation add new layers of stress. The European Journal of Preventive Cardiology projects that cardiovascular disease mortality will continue to rise globally through 2050 unless urgent preventive measures are taken.
The current situation is unsustainable. Bangladesh’s rising temperatures and frequent climate disasters are not only worsening physical health but also amplifying mental distress. The World Heart Federation’s 2025 report emphasizes that noncommunicable diseases, including cardiovascular stress, are now the dominant global health challenge. At the same time, WHO data show that mental health conditions affect people of all ages and income levels, with suicide accounting for one in every 100 deaths worldwide.
Recommendations must be bold and actionable. First, integrated public health campaigns are essential to raise awareness about hypertension, healthy diets, and stress management. These campaigns should be culturally tailored and reach rural as well as urban populations. Second, strengthening primary healthcare systems is critical. Routine blood pressure checks, affordable medications, and counseling services should be made widely available. Third, mental health must be destigmatized through education and policy reforms. Training community health workers to provide basic psychological support can bridge gaps in mental health infrastructure. Fourth, climate adaptation strategies must be linked to health planning. Cooling centers, green spaces, and urban design that mitigate heat stress can reduce both cardiovascular and mental strain. Fifth, global cooperation is needed. International organizations should support low-income countries like Bangladesh with funding, technology transfer, and expertise to combat these dual crises.
The socio-public health impacts of cardiovascular and mental stress are not confined to hospitals; they permeate schools, workplaces, and homes. Governments must recognize that investing in preventive health is not a luxury but an economic necessity. Bangladesh stands at a crossroads. With one-third of deaths linked to heart disease and rising mental health burdens, the country cannot afford piecemeal interventions. A comprehensive national strategy that integrates cardiovascular and mental health into broader development goals is imperative. Globally, the same lesson applies: health systems must evolve to address the intertwined nature of physical and psychological stress.
In conclusion, cardiovascular and mental stress are silent epidemics reshaping public health landscapes in Bangladesh and worldwide. Their causes are deeply rooted in modern lifestyles, environmental changes, and systemic inequities. Their impacts extend beyond individual suffering to national economies and social cohesion. The evidence from Bangladesh’s rising heart disease rates, climate-induced mental health challenges, and systemic stressors paints a clear picture: urgent, integrated action is required. Recommendations centered on awareness, healthcare strengthening, destigmatization, climate adaptation, and global cooperation offer a path forward. Without such measures, the dual burden of cardiovascular and mental stress will continue to erode health, prosperity, and resilience across societies.
Author: Dr. Md. Aurangzeb, a seasoned public health expert with two decades of experience, is an educator, author, and media commentator. Specializing in environmental health, WASH, solid waste management, policy reform, and humanitarian initiatives, he advocates impactful solutions to global health challenges.